Cannabis Does Not Reduce Pain, It Makes It More Bearable
Last updated on Tuesday 18 June 2013
Originally published on Monday 24 December 2012
http://www.medicalnewstoday.com
Cannabis Does Not Reduce Pain, It Makes It More Bearable
Using cannabis for pain relief does help, however, it makes pain more bearable rather than getting rid of it, researchers from Oxford University’s Centre for Functional Magnetic Resonance Imaging of the Brain (FMRIB) reported in the journal Pain.
The authors added that people in pain act differently to cannabis, according to their brain imaging study.
The principal psychoactive constituent of cannabis is called tetrahydrocannabinol (THC). The researchers found that when volunteers took oral tablets of THC, they tended to find the experience of pain more tolerable. There was no evidence that THC reduced pain intensity.
Several studies have found that cannabis is associated with some kind of improvement in pain symptoms. Researchers from McGill University Health Centre (MUHC) and McGill University reported in CMAJ in 2010 that patients with chronic neuropathic pain experienced pain relief, improved mood and better quality sleep after smoking cannabis.
Scientists from Imperial College London found that Cannador, another cannabis plant extract, effectively relives pain after major surgery. They reported their findings in the journal Anerthesiology.
Researchers from the Mayo Clinic, however, said medical marijuana is not recommended for teenagers with chronic pain.

THC is one of 400 compounds found in the Cannabis plant
According to MRI brain imaging scans in this latest study, areas of the brain that interpret pain were not affected significantly when people took THC. It appears that cannabis affects people’s emotional state in a way that makes pain less awful.
Lead researcher, Dr Michael Lee, said:
“We have revealed new information about the neural basis of cannabis-induced pain relief. Cannabis does not seem to act like a conventional pain medicine. Some people respond really well, others not at all, or even poorly. Brain imaging shows little reduction in the brain regions that code for the sensation of pain, which is what we tend to see with drugs like opiates. Instead cannabis appears to mainly affect the emotional reaction to pain in a highly variable way.”

Health care professionals and administrators say that chronic (long-term) pain is a complex healthcare problem. In order to help patients effectively manage their pain, different approaches are needed, which can include physical therapy, psychological support, and medications.
For a number of patients who have not responded adequately to drugs, cannabis or cannabis-based medications are an effective way of controlling their pain. Many, however, report no benefits from cannabis and some undesirable side effects.
Dr. Lee said “We know little about cannabis and what aspects of pain it affects, or which people might see benefits over the side-effects or potential harms in the long term. We carried out this study to try and get at what is happening when someone experiences pain relief using cannabis.
Our small-scale study, in a controlled setting, involved 12 healthy men and only one of many compounds that can be derived from cannabis. That’s quite different from doing a study with patients. My view is the findings are of interest scientifically but it remains to see how they impact the debate about use of cannabis-based medicines. Understanding cannabis’ effects on clinical outcomes, or the quality of life of those suffering chronic pain, would need research in patients over long time periods.”
Dr. Lee and team carried out several MRI scans on 12 participants at the FMRIB center in Oxford, England.
The volunteers were divided into two groups:
• The THC group – participants were given a 15 mg THC tablet. THC is one of 400 different compounds found in the cannabis plant. It is the one that gives recreational smokers the “high”.
• The placebo group – the participants were given a dummy drug that looked just like the tablet those in the other group were taking
Then the groups were swapped, so that each participant eventually had been tested with THC and placebo.
The volunteers had either 1% capsaicin cream rubbed on the skin of one leg, or a dummy cream. Capsaicin is the ingredient of chillies; when rubbed on skin it causes a burning, painful sensation. Then the ones who received the dummy cream received the 1% capsaicin cream and those that had received the pain-inducing cream received the dummy cream.
In all, each participant underwent four situations:
• They took a THC tablet and had the pain-inducing cream applied to their skin.
• They took a THC tablet and had the dummy cream applied to their skin.
• They took a placebo tablet and had the pain-inducing cream applied to their skin
• They took a placebo tablet and had the dummy cream applied to their skin
In each different situation they had an MRI scan – a total of four scans per participants.
They were asked to describe the intensity and unpleasantness of their pain in each situation. The volunteers had to describe how intense the burning sensation was, and how much of a bother the pain was.
They found that with THC, many of the volunteers said the pain bothered them less, but did not report any change in the burning sensation.
Even though their findings showed that THC’s average effect was statistically significant, people’s reaction to pain after taking the compound varied considerably. Half of them reported a “clear change in how much the pain bothered them.”
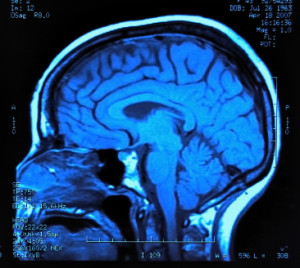
The participants’ reports regarding how unpleasant their pain was were backed up by MRI scan results. An area in the bran called the anterior mid-cingulate cortex, which has many functions, including the emotional aspects of pain, became less active after participants took THC.
The scans also showed that activity changed in the right amygdala, which correlated with the reduction in the unpleasantness of the pain after people had taken THC. Experts already know that pain can “prime” the right side of the amygdala.
The scientists were particularly interested in how closely the right amygdala and the primary sensorimotor area (a part of the cortex) were connected. The strength of the connection between these two brain areas correlated well with the THC’s varying effects on the pain the participants had reported.
The scans may help doctors predict who may benefit from taking cannabis for the relief of pain, the authors wrote.
Dr. Lee said:
“We may in future be able to predict who will respond to cannabis, but we would need to do studies in patients with chronic pain over longer time periods.”
Written by Christian Nordqvist
Copyright: Medical News Today
http://www.medicalnewstoday.com